Waist deep in the Big Muddy
Gov. McKee’s administration halts its $7 billion contract bidding process for Medicaid’s managed care organizations
We live in such a small world, particularly here in Rhode Island, where the numbers of health care reporters are few. The willingness to dig deep into the often dense material surrounding the issues around health care – such as being able to talk in complete sentences that make sense about accountable entities – is a skill that requires more than just reporting on the facts and figures.
It is about capturing the stories that go with the numbers, doing justice in covering the personal stories of our lives, which are our most valuable possessions.
PROVIDENCE – It was as if the state of Rhode Island had finally woken up in the middle of a nightmare of its own making.
On late Friday afternoon, May 13, the R.I. Department of Administration under Gov. Dan McKee announced that it was canceling the bidding process for re-procurement of the state’s managed Medicaid contract, said to be worth $7 billion over five years.
The question remained: How many folks were going to keep singing along, joining in with the chorus of the infamous Pete Seeger ballad, …“We were waist deep in the Big Muddy, and the big fool said, ‘Push on.’”
Under the contract, private health insurance firms were to be chosen to deliver health care benefits to approximately 85 percent of the nearly 350,000 Rhode Islanders enrolled in Medicaid.
Currently, there are three such private health insurers – Neighborhood Health Plan of Rhode Island, UnitedHealthcare, and Tufts Health Plan – working under the contract that expires as of July 1, 2023.
However, Tufts Health Plan, a division of Point32Health, was disqualified from the re-procurement process, allegedly for having delivered its paper application for the bid a few minutes after the deadline.
Then, as WPRI reported, another bidder in the procurement, Blue Cross and Blue Shield of Rhode Island, had apparently delivered a disk that was blank as part of the application process.
After weeks of apparent disagreement, with the R.I. Executive Office of Health and Human Services urging the R.I. Department of Administration to halt the process, but the R.I. Department of Administration allegedly refusing to do so, the McKee administration apparently decided to halt the bidding process and to begin again.
“This is wild,” declared WPRI’s Ted Nesi on Twitter, talking about the decision to halt the procurement.
Were the warning signs missed?
There were plenty of warning signs that, much like Miss Clavel, a character in the children’s story, “Madeline,” had said: “Something is not right.”
• The abrupt departure on May 1 of Secretary Womazetta Jones, from the R.I. Executive Office of Health and Human Services, without a clear reason being given. Jones had been serving as the point person coordinating the re-procurement process. [See link below to ConvergenceRI story, “Through a lens of racial equity.”]
During an interview conducted by ConvergenceRI with Secretary Jones in early February which had preceded the announcement of her departure, Jones told ConvergenceRI she had been surprised to learn about the content of testimony during the special Senate legislative commission hearings on the future structure of R.I. EOHHS, information that apparently had not been accurately relayed to her.
• The role that the R.I. Department of Administration played in disqualifying Tufts Health Plan from the bidding process, because of an alleged late paper application. The disqualification of Tufts Health Plan effectively put an end to the experiment known as the “Reinvention of Medicaid.” [See link below to ConvergenceRI story, “The big disconnect.”]
Apparently, the case of the late application involving Tufts Health Plan was not the only time that the R.I. Department of Administration had become involved in a controversy over an alleged late application for a state contract. The application by Doctors Test Centers, the firm co-owned by Republican candidate for Governor, Ashley Kalus, for a contract to administer COVID-19 tests and vaccines in Rhode Island, was initially deemed ineligible because of being late, but that disqualification was later overruled and the firm was awarded the contract, according to news reports.
• The bloated Medicaid rolls for Rhode Islanders, which, as of March 31, 2022, stood at 347,977, according to Kristin Sousa, the new director of the R.I. Medicaid office. [See link below to ConvergenceRI story, “Meet the woman in charge of Medicaid in RI.”]
If and when the federal government lifts its emergency COVID declaration, as many as 50,000 Rhode Islanders may lose their health insurance benefits, because of eligibility determinations which were halted during the pandemic.
• The continuing controversy over the failure – by the Medicaid office, by Gov. McKee’s administration, and by the R.I. General Assembly – to increase the Medicaid reimbursement rates, many of which have not been increased in more than a decade.
The failure to raise reimbursement rates has been linked to many of the ongoing crises in mental health and behavioral health care services, the health workforce, and the fact that Early Intervention services were shut down. [See link below to ConvergenceRI story, “Is there a news credibility gap in RI?”]
• The questions raised concerning the potential conflict of interest about the role of Optum, a wholly owned, for-profit subsidiary of UnitedHealthcare, in managing the benefits for both Neighborhood Health Plan of Rhode Island and UnitedHealthcare, the two largest current managed care organizations serving Medicaid members in Rhode Island.
On the commercial side of the insurance business, UnitedHealthcare [and Optum] were recently fined by the R.I. Office of the Health Insurance Commissioner for their failure to abide by mental health parity laws in Rhode Island. [See link below to ConvergenceRI story, “The problems with Optum continue.”]
Further, there is a news conference scheduled for Monday morning, May 16, at which R.I. Attorney General Peter Neronha is expected to announce that Rhode Island will be joining legal action in an appeals court case against UnitedHealthcare, in support of the state’s mental health parity laws.
At the same time, the tentacles of Optum’s reach in the health care market continue to grow, with the recent announcement that Optum is seeking to acquire Atrius Health, the largest independent physicians network in Massachusetts, a group reported to include 715 physicians, for $236 million. Massachusetts AG Maura Healey signed off on the deal in April.
• There is the continuing controversy/scandal regarding Eleanor Slater Hospital and its eligibility to receive Medicaid funds. Each new chapter in the sordid story keeps getting darker – the apparent release of a patient without any continuum of care plans, allegedly contributing to the patient’s death. [Kudos to Kathy Gregg, reporter with The Providence Journal, and to Eli Sherman at WPRI, in being persistent in pursuing this story.]
The underlying problem remains the same: Whether or not the hospital system managed by the R.I. Department of Behavioral Healthcare, Developmental Disabilities, and Hospitals is eligible to receive federal Medicaid funds to cover the care for patients with long-term mental health issues.
Translated, the goal of the McKee administration, under the direction of R.I. BHDDH Director Richard Charest and the agency’s chief medical officer, Dr. Elinore McCance-Katz, seems to be to avoid the liability of having to increase the state’s Medicaid expenditures by as much as $40 million, because of an imbalance in the patient population at the hospital.
Tilting at windmills
At the State House, community advocates have been vocal and persistent in seeking remedies, demanding increases in Medicaid reimbursement rates and, more importantly, an end to what they have described as “a top-down process driven by external consultants,” preserving the status quo of the current bureaucratic power relationships under R.I. EOHHS and R.I. BHDDH.
“There are thousands of Rhode Islanders with serious and persistent mental illness and substance use concerns,” Benedict Lessing, Jr., MSW, President and CEO of Community Care Alliance, wrote in a recent email to his colleagues, arguing against the state’s proposal to spend $28 million on its own version of Certified Community Behavioral Health Clinics, rather than following the federal guidance. “Absent immediate Medicaid rate increases or a commitment of additional funding for stabilization purposes, we will see these populations encounter increased contacts with law enforcement, corrections, child welfare and hospital systems.”
The problems with Medicaid in Rhode Island
With the apparent re-opening of the state bidding process for procurement to select private health insurance firms to manage the health care benefits for more than one-third of Rhode Island’s population on Medicaid, the opportunity to pose some larger, fundamental questions may begin to re-emerge. They include:
• Does there need to be audits conducted on the three health insurance firms that are currently serving as the MCOs for Medicaid in Rhode Island?
• How are “shared savings” divvied up by the health insurance firms serving as MCOs for Medicaid in Rhode Island, as part of the “accountable entity” program? In particular, how much of any “shared savings” went to the health insurer, how much went to the state, and how much went to the actual accountable entity – the providers such as community health centers doing the work?
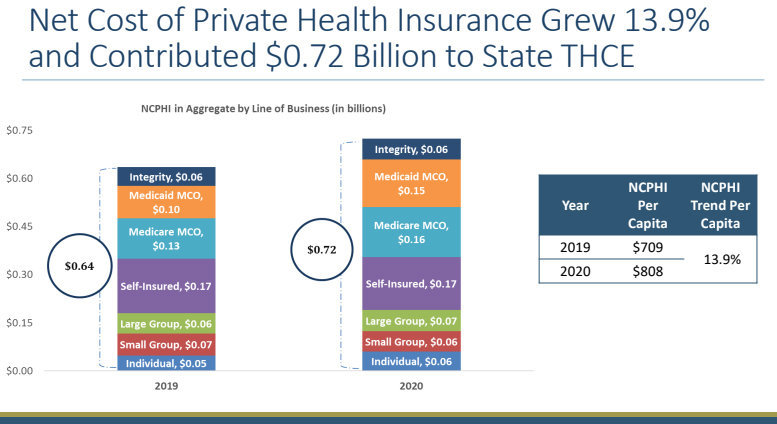
Further, the recent data analysis published by the RI Health Cost Trends Steering Committee, analyzing the state health industry sector’s “Performance Against the 2020 Cost Growth Target, conducted by Bailit Health at the direction of the R.I. Office of the Health Insurance Commissioner, provides great opportunities to begin to ask questions about the value – the return on investment – on what amounted to $8 billion in health care spending in 2020. [See links below to ConvergenceRI stories, “The bigger disconnect,” and “Distraction rules: Are $8B in annual health costs the ‘third rail’ in RI politics?”]
With the announced departures of both Dr. Timothy Babineau, president and CEO of Lifespan, and Dr. James Fanale, president and CEO of Care New England, the opportunity exists, perhaps, to open up the dialogue around the role of “leadership” in Rhode Island – by elected officials, by government regulators, and by public-private partnerships – to look at solutions to improve the ever-increasing costs of delivering health care in Rhode Island.
ConvergenceRI had reached out to Anya Rader Wallack, who now serves as senior vice president at the University of Vermont Health Network, to get her feedback on the latest cost trends analysis. [Previously, Rader Wallack had served as the associate director of the Center for Evidence Synthesis in Health and a professor of the Practice in the Department of Health Services, Policy and Practice within Brown University’s School of Public Health. In addition, she had served acting secretary of the R.I. Executive Office of Health and Human Services, director of the R.I. Medicaid office, and director of HealthSource RI, the state’s health insurance exchange.]
Translated, Rader Walllack is an expert with a great deal of expertise when it comes to talking about health care costs and data analytics.
ConvergenceRI: Rhode Island is launching a new statewide compact, a value-based payment compact for new payment models, focused on cost containment. Does there need to be further work done on defining “value” as something different than measuring and reducing costs?
RADER WALLACK: Leadership commitment is incredibly important, so I am impressed that Rhode Island leaders have taken this most recent step. Defining and redefining value is really important and should be a never-ending process.
I don’t know anyone who defines value as simply reducing costs – there has to be a denominator – cost per what? Cost relative to health care outcomes, relative to population health, relative to health equity – all fronts on which we should measure and continually refine our measurement and evaluation.
ConvergenceRI: What role should patients play in defining the parameters of health care delivery systems around continuity of care?
RADER WALLACK: Patients should be at the center of this. Nobody sees the gaps, strengths, and weaknesses in care better than them. But then we need to translate their experience to things we can measure and improve upon.
ConvergenceRI: From Vermont’s experience, how can a state seek to create a system of health care that aligns with a collaborative approach?
RADER WALLACK: First and foremost, a state should try to get providers and payers to work together, as Rhode Island appears to be doing. Vermont has done this well in the past, but there is less alignment now.
Competition between providers and payers around who can control health care costs is stupid. None of us know the answers, but all of us have an interest in finding the answers.
ConvergenceRI: What role should data analysis play in decision-making around health care cost trends?
RADER WALLACK: Data analysis should be the foundation for this work. It’s hard to find good data to compare costs and quality state-to-state on an all-payer basis, but this should be the goal. If we aren’t all striving to agree upon the “truth” in the available data, we will argue over incomplete information and get nowhere.