The bigger disconnect
The latest data analysis by the RI Health Cost Trends Steering Committee for 2020 indicates that because of COVID 19 and large infusions of federal funding, the data outcomes may be considered as an anomaly
In the settlement with Teva, announced on Tuesday, March 22, Teva agreed to supply Rhode Island with supplies of Naloxone and Suboxone that are sufficient to meet the state’s projected needs for the next 10 years, according to state health officials. The supplies include 50,000 kits of Naloxone [100,000 nasal sprays] valued at $62.5 million, and Suboxone medication valued at $16 million over 10 years.
In total, Attorney General Neronha’s aggressive pursuit of opioid manufacturers, distributors, and consultants has resulted in more than $250 million to support opioid treatment, rescue, prevention and recovery in Rhode Island.
PART Two
PROVIDENCE – The common wisdom for many is that if you cannot measure it, the work does not get done. But what happens when the standard measurement tools that are being used to assess and analyze the growth of health care costs in Rhode Island on an annual basis become, like a ship that has lost its mooring during a storm, set adrift?
On Tuesday morning, March 29, the RI Health Care Cost Trends Steering Committee will officially release its analysis of the industry sector’s “Performance Against the 2020 Cost Growth Target,” conducted by Bailit Health consultants.
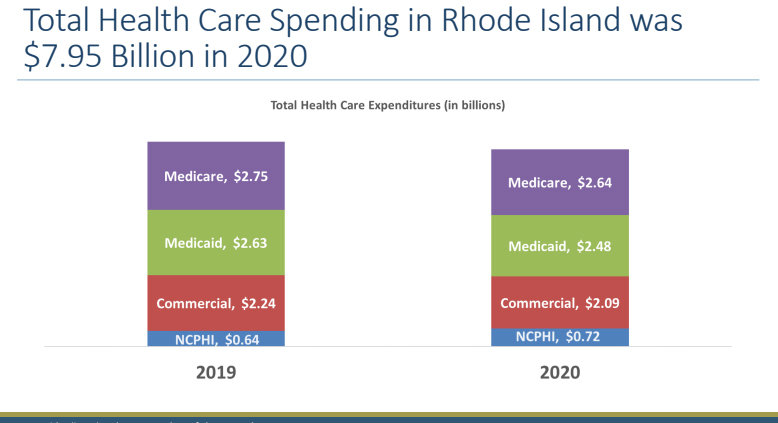
The data for 2020 showed that almost all of the existing spending targets for an annual 3.2 percent increase in expenditures were met, and that health care spending in Rhode Island decreased by 3.1 percent, to $8.921 billion in 2020, compared to $9.210 billion in 2019.
But, any conclusions drawn from the data require a number of caveats. The problem, as the 51-page report acknowledged at the beginning of the document: “The 2020 reporting year was unique because of aberrant health care utilization [emphasis added] and spending due to the global COVID-19 pandemic.”
How steep was the drop in utilization in 2020? OHIC found that inpatient admissions dropped 6.2 percent in 2020 in the commercial insurance market, and as much as 8.1 percent in the individual insurance market, based on last year’s rate filings by health insurers.
Factors that contributed to the drop in utilization in 2020, according to the trends analysis, included
• A significant reduction in health care service utilization due to postponement of elective procedures and patient reluctance to access care.
• A significant increase in telehealth visits in Rhode Island.
The trends analysis said that health insurance plans were required by both the R.I. Office of the Health Insurance Commissioner and the R.I. Executive Office of Health and Human Services to pay for telehealth visits for certain service codes with no cost-sharing requirements. Further, the agencies mandated the equivalency of payment between telehealth and office visits.
Other factors that may have skewed the data results, according to the trends analysis, were an influx of federal funds to providers. These included:
• Approximately $580 million paid to Rhode Island providers in COVID relief funds in 2020 under the CARES Act.
• Separately, R.I. EOHHS reported disbursing nearly $275 million in COVID-related funds in 2020, including $220 million under the Hospital Assistance Partnership Program.
Translated, any data analysis of cost trends for 2020 was filled with factors that would make comparisons to previous years – and future years – problematic.
As the trends report summarized, “While the analysis found that per capita spending went down, the large volume of federal spending for which we could not account in our calculations brings into question the accuracy of this finding.”
Melanie Coon, managing director of Corporate Communications at Blue Cross and Blue Shield of Rhode Island, said that the data results from both 2020 and 2021 may prove to be skewed by the COVID pandemic.
"Clearly the pandemic was a factor in the 2020 spending decreases across the board," Coon said, in an email to ConvergenceRI. "Many folks postponed elective procedures and were reluctant to access care in the midst of lockdowns and other pandemic protocols."
"We expect 2021 will be another anomaly, also due to the pandemic," Coon continued. "It's also important to consider that federal health care expenditures in response to COVID-19 are not incorporated into the cost trends analysis."
Coon also noted that "prescription drugs are the largest driver of cost growth," a key trend identified by the cost trends analysis.
Data trends that stuck out
At the same time, there were some compelling trends identified within the trends analysis for 2020. They included:
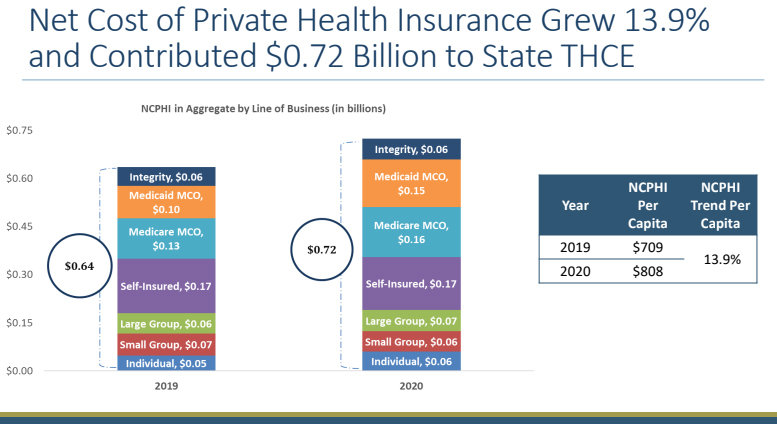
• The “Net Cost of Private Health Insurance” grew by 13.9 percent in 2020, compared to 2019, and contributed approximately $720 million to the state’s total health cost expenditure, despite the reduction in utilization in 2020.
The largest increase in health insurance costs were from the Medicaid MCOs, or managed care organizations, which grew by 41 percent. This increase is particularly noteworthy, given the current re-procurement underway by the state for MCOs for Medicaid. [See link below to story in ConvergenceRI’s current edition, “The big disconnect.”]
The next two highest categories were the individual market, where costs rose by 26 percent, and in the dually eligible segment [Medicare and Medicaid], for the “Integrity” program, where costs rose by 25 percent. Neighborhood Health Plan of Rhode Island is the sole contractor for the Integrity program.
Another fascinating bit of data analysis was the fact that the trends analysis could not determine whether or not Neighborhood Health Plan of RI’s performance as a “commercial health insurer” had met the target of a 3.2 percent annual increase in spending.
Drugs, drugs, drugs
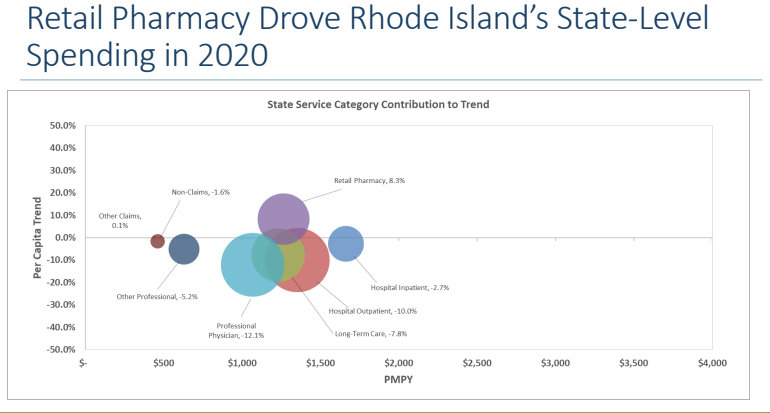
The one consistent factor in both 2019 and 2020 analyses was the way that retail pharmacy costs drove increases in Rhode Island’s medical spending – in the commercial market, in the Medicaid market, and in the Medicare market.
As the report summarized: “Retail pharmacy spending continues to be a significant cost growth driver in Rhode Island and a threat to the state’s future cost growth target attainment.”
To infinity – and beyond
In looking to what the cost analysis trends might show for 2021 in terms of utilization, with a promised rebound, the other unknown factor is how the health care industry will account for the growing number of conditions apparently related to COVID-19 infections, including “Long COVID” and other conditions that have arisen, including a steep rise in the incidence of Type 2 diabetes, reported problems with ongoing damage caused to different body organs, including the brain and the kidneys, and potential behavioral health conditions attributed to COVID infections.
“We certainly need to “asterisk” the year 2020, considering the context of the pandemic,” said State Sen. Lou Di Palma, when asked for his initial response to the Cost Trends Analysis. “We, the state of Rhode Island, along with each state in the union, received significant federal funds, which clearly added to the overall dollars spent,” Di Palma continued.
Di Palma also cited the increasing costs of retail pharmacy. “Additionally, as we know and is confirmed in the report – ‘Retail pharmacy spending continues to be a significant cost growth driver in Rhode Island.’” Di Palma continued: “It is critically important we address and reverse the ever-increasing rising drug costs. There are several pieces of legislation seeking to once and for all address this.”