“The more we do what Big Pharma wants, the higher the costs are going to be”
Blue Cross and Blue Shield of RI talks about the levers it is deploying to try and reduce high pharmacy costs
The reality is that the COVID virus will continue to mutate, with each new variant seeking out the vulnerabilities of our collective immune system. If the R.I. General Assembly were truly interested in jumpstarting bio-manufacturing industry sector in the state, they would configure an investment bank to support the work being done by De Groot and her team. The issue is not about creating more wetlabs, but rather creating the financial resources to speed vaccine development and personalized cancer care.
PROVIDENCE – The truth and consequences surrounding how Big Pharma spends billions of dollars a year on advertising and marketing in order to persuade consumers and doctors to choose their high-priced drugs for treatment is no hidden trade secret.
The continuing legal battles over the Sackler family’s pursuit of its fortune, based upon its addictive prescription painkiller, OxyContin, has achieved news notoriety. The saga has been made into a stirring Hulu series, “Dopesick,” based on the reporting by Beth Macy.
The Empire of Pain: The secret history of the Sackler Dynasty, written by Patrick Radden Keefe, retells the sordid tale in great detail of how the Sackler family enriched themselves by evading accountability, federal regulation and law enforcement.
And, the latest book by Sam Quinones, The Least of Us: True Tales of America and Hope in the Time of Fentanyl and Meth, explores the darkness at the edge of town in almost every American community, as the nation continues to move through its dystopian love affair with illicit drugs.
Here in Rhode Island, Attorney General Peter Neronha has been a leader in the legal fight to try to hold Purdue Pharma and the Sackler family accountable, on the winning side of a successful appeal to a federal district court judge that threw out an earlier bankruptcy court settlement.
Neronha also won a lawsuit in 2021 against McKinsey & Company for its role in “turbocharging” the opioid epidemic on behalf of the Sacklers and Purdue Pharma. A trial in federal court against the three distributors is now scheduled to begin in March of 2022 in Providence.
What may be a bit surprising for many, then, is the growing recognition by the state’s largest health insurance firm, Blue Cross & Blue Shield of Rhode Island, voicing its growing alarm about the need to better control increasing pharmacy costs, which are the leading driver of higher health costs in the state.
Listen to how Martha Wofford, the president and CEO of Blue Cross, described the current reality, in an exclusive interview with ConvergenceRI:
“I know you know this; pharmacy is the biggest driver of increased health care costs, but I thought we would spend a little time talking about it as a problem,” Wofford began.
The interview with Wofford was the third in a series of conversations with ConvergenceRI conducted in the last seven months, during each of which a part of the discussion focused on the reasons behind why pharmacy costs had emerged as the major driver of increased health care costs in Rhode Island.
At Wofford’s request, following the second interview in November of 2021, a third session was set up to discuss specifically the rise in drug costs and what could be done to better control them.
Laying the blame on Big Pharma
Wofford did not mince words about the root causes behind the increased health care costs. “Pharmacy now makes up a third of all health care costs,” Wofford said, setting the table for the conversation. “And specialty pharmacy is now over 50 percent of that total pharmacy spend.”
Wofford continued: “When we say specialty pharmacy we are talking about a small number of very expensive drugs. These drugs have huge variations in cost from drug to drug, and quite incomplete quality information.”
The news got worse. “I was actually alarmed when the team shared this data point with me – that for Blue Cross [and Blue Shield of RI], 1 percent of our pharmacy claims equals 50 percent of our pharmacy spend.”
The culprit behind in the rising pharmacy costs is Big Pharms, Wofford said, sounding a bit more like a consumer advocate and not the president and CEO of the state’s largest commercial health insurance firm.
“I just saw a study about how Abbvie, the manufacturers of Humira, spent $1.5 billion on advertising for Humira over a three-year period,” Wofford said. “I think Humira is an example of big price increases – a 10 percent increase last year, with no change in the drug.”
This kind of dramatic price increase, Wofford continued, “is allowed to happen only because Big Pharma spends so much money on lobbying, more than any other industry,” expressing her exasperation at the outsized role that Big Pharma plays in lobbying Congress, enabling it to hike drug prices unfettered.
Here is the ConvergenceRI interview with Martha Wofford, president and CEO of Blue Cross & Blue Shield of Rhode Island, and Chris Bush, senior vice president of Network Management and Pharmacy Operations, focused on strategies the insurer is pursuing to control rising pharmacy costs.
ConvergenceRI: Thank you for setting the table for our discussion today.
WOFFORD: In the U.S., I know there is a lot of conversations about the need for these high prices to fund the R&D, but if you actually look at where [Big Pharma] spends their money, most of it is actually being spent on marketing and advertising, versus research and development. A lot of the R&D investment actually comes from the National Institutes for Health and is taxpayer-funded.
The other thing that I wanted to share is [the fact that] not only is specialty pharmacy growing at alarming rate, but there is quite a pipeline of new drugs out there.
BUSH: As a contextual reference, there are 400-plus approved specialty medications in the market today, and that compares to about 30 back in the 1990s.
So, that explosiveness has certainly added to the number of available drugs. Just in comparison to 2020, we have had a four-times increase in the high-cost drug therapies entering the market.
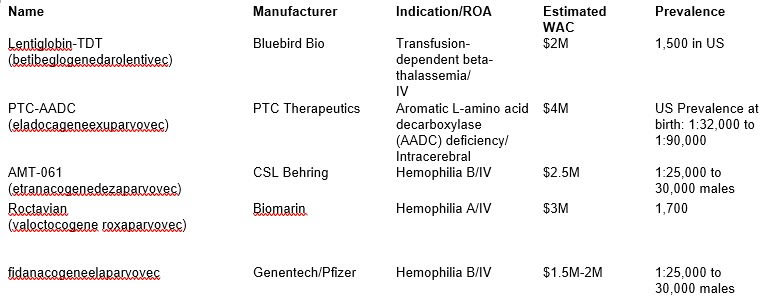
And, projecting into 2022, we have five new drugs that are expected to be priced at or above $1 million.
ConvergenceRI: What drugs are those?
BUSH: I can provide the names, if you’d like, afterwards. [See third image above.]
ConvergenceRI: I tried to monitor the news of what was coming out of the JP Morgan health conference last week, which is the trendsetter when it comes to discussions around health care investments. I was surprised, if that is the right word, that the CEO of Biogen, Michael Vounatsos, admitted that the company had been wrong to price its Alzheimer’s disease treatment drug at $56,000 a year, and called the decision to cut the price in half “courageous.”
What it says to me is that there are no adequate controls over how drug companies price their products. And, the federal government is struggling with how to control costs. Could you address how do we shift the momentum to achieve more accountability?
WOFFORD: That is a great question. I think it is the right question. We have three levers that we are employing right now. I wouldn’t say that we are changing the dynamics as much as we would like to hold them accountable.
The three levers, let’s just take them in turn: The first one is improving how we manage drugs. One of the things that we do here in Rhode Island is that we embed pharmacists into primary care physician [PCP] practices. And that is because it has gotten very technical and very hard for a primary care physician to manage the complexities of so many of these drugs.
This is an investment that we made to help all patients, not just Blue Cross members. We also do things like push generics and lower-cost drugs, which is another key lever.
And, I know no one likes going through Step Therapy, but the reality is, branded drugs are five times as expensive as generics, on average.
And, sometimes patients want a specific drug, because of the advertising we have seen, or because our physician might be more familiar with the more expensive drugs, because those are the drugs that Pharma reps talk to them about to try and influence their prescribing choices.
I am a huge advocate for primary care physicians, and it is by no means their fault, or the specialists’ fault, when they get influenced in choices by these Pharma reps.
It is also the case that the evidence base [for drugs] is moving at this incredible pace. There is no way that your average PCP could read the dozens and dozens of articles that they would have to do every day, to try and stay up to date for what the best therapeutics are.
The other lever, on the management side, that we try to focus on is integrated pharmacy benefits with medical benefits, to manage the patient holistically by managing both their pharmacy and medical needs.
BUSH: We look at the cost of the drug, but also the utilization and efficacy of the drug, something we closely monitor.
The embedded pharmacists that we have within our ACO [accountable care organization] agreements certainly help to do that.
But there are also opportunities to utilize some of the local distribution channels, in partnership with hospitals.
They have a whole host of clinical pharmacists that are embedded at a condition-specific level, so if you think about oncology, that specialty, you have pharmacists that are aligned, really watching the adherence and the outcomes, and whether the drugs are producing the effective results that the doctor is intending to see. And they are following up with those patients on a regular basis.
And, if there appears to be something that is outside of what the normal outcome or course of treatment would be, whether it is an adverse effect, or progression, they are monitoring that, and then they have frequent and regular contact with that prescriber to alter that medication.
ConvergenceRI: Many of the new specialty drugs that being prescribed are drugs delivered through infusion. Is that accurate? Has that resulted in an influence on drug costs, drug prices, and the costs of methods of delivery?
BUSH: I would say absolutely that that is a trend that we are seeing. I would also say, in general, the infused products are covered under our medical benefits.
Not only is it the cost of these drugs that we watch closely, but it is also where the infusions are being provided. We are looking at access to care, the ability to deliver those products to members on a regular basis. This is where we look at the total cost of care across an episode.
The same principles apply; we would evaluate the drug that is being distributed or disbursed, asking: is it consistent with the condition, the dosing and the cost that we have established?
Secondary to that, from a model standpoint, you might have drugs being infused in a hospital setting, which may not be the most appropriate setting, whether it is because of travel time or convenience. This is where alternative sites may come into play. We have established locally in the market opportunities for members to visit free-standing infusion standards.
Which are typically more convenient, offer expanded hours, and in some instances, infusions can occur at home.
And with each of those options, we are trying to address the cost delivery of the drug, but also member convenience as well.
WOFFORD: There is another lever we have to try and control pharmacy costs, which is how we buy drugs. We are partners in something called Civica Rx, which is a consortium of hospitals we are working with to bring “biosimilars” to market. Big Pharma has often sought to block them, so we are working with different manufacturers to bring biosimilars to market, so we are not completely dependent on those branded options.
We are also working very hard to collect the most cost-effective drugs for our formulary. As you may be aware, many of these new, very expensive drugs don’t have the clinical evidence to support their efficacy.
With Alduhelm [the new Biogen Alzhemier’s drug], it is a very expensive drug that didn’t have clear clinical results in trial, and yet it was brought to market.
We have the ability where there is more than one therapy, which is not the case everywhere, to actually pick a winner in that category, that can start to bring down the costs to consumers.
BUSH: A good example would be drugs used to treat advanced macular degeneration. If we take a look at the therapies that are in that category, you have a drug that has been around for a while, that has produced great outcomes, in Avastin, and a cost that averages about $50 per injection.
And, there is a competing drug, one that is newer to market, Lucentis. In comparison, it has similar efficacy and outcomes, but the cost of that drug is over $2,000 an injection.
WOFFORD: What happens, Richard, is that you have patients who cannot afford that much higher price tag, because they are paying co-insurance for those drugs. There was a whole strategy that tried to make Avastin unavailable for opthalmologists to use, once they actually had Lucentis available to market.
There is a lot that Big Pharma does to try and drive the more expensive drug to be the one most available. So, we pursue counter measures to try and select the drugs that have similar outcomes but are much less expensive.
Another lever in the category of buying drugs is how can we get to an outcomes-based agreement. During our last interview, you and I talked a bit about value-based care as the direction we need to go in as a health care system.
In my opinion, this is a space in which we can start to measure outcomes, and then really push Big Pharma to put their money where their mouth is. And say, if this is such a great drug, then are they willing to be at risk for the results of using it? And we are more than willing to have those kind of agreements for some of these new therapies.
ConvergenceRI: Is there a role for the state to become involved in all of this, in what might be termed buying cooperatives. I know that there is, around vaccines, for instance, the state has joined with other states to buy drugs as a consortium. Is there a similar approach for the state to get involved? Or would you prefer that they not get involved?
WOFFORD: There absolutely is an opportunity. One of the things that we have been talking to legislators about is actually creating a fund for high-cost, what we call orphan drugs, so that you can pool together the patients who need them and their purchase.
Because what happens is that an individual employer may have one or two patients who need these life-saving medications. But, if you are a small employer, it can be really, really challenging to cover those costs. What we are trying to do with this fund is spread those costs across the state.
Also, if you have a larger number of patients, you can go to the manufacturer and try to get a better rate, because you have some of that scale.
There is absolutely a role for the state, and in fact, other states are doing things that we are not doing yet.
New Hampshire actually passed a ban on the sale of prescription data, which Pharma companies had been tracking for years, to learn what the physicians actually do and who they can try to contact to increase their sales in terms of prescribing.
There is also work being done to require transparency on some of the sorts of Pharma reps in other states.
I know that you have reported on quite a bit the Purdue Pharma OxyContin cases and the opioid crisis. There is a very dark role that some of the Pharma reps played in influencing the opioid crisis, and I think there is quite a good opportunity on different fronts for the state to play a more activist role.
BUSH: If I can just add some other examples in neighboring states as well, regarding the inflationary costs that drug manufacturers seek to pass on each year. There are states right now that regulate that amount of price increase. For example, saying that a manufacturer could not pass along a 10-percent increase in costs within a 12-month period.
ConvergenceRI: How can you address the barrage of advertisements pushing specialty drugs? How can that be reined in?
WOFFORD: I agree with you. And, I believe we are only one of two countries in the world that allows such advertising [the other is New Zealand]. It is something that we should address, but I would say, after watching how challenging it was to get any kind of changes in drug policy through legislation in Washington, I don’t know what path exists to make a change there, because the Big Pharma lobby is just so powerful.
ConvergenceRI: How do we reset the marketplace in terms of information, and the challenges we face in trying to communicate accurate information about drug costs?
WOFFORD: I really appreciate you question. I think covering the story for your readers makes it more understandable. Because the more we do what Big Pharma wants, the higher the costs are going to be. Those costs go somewhere, and increasingly, it gets borne by individual consumers.
We have to arm our customers and to arm our physicians and partners to face all of this, while we work on how do we improve the way we buy drugs in the most efficient way we can.
I take your question to heart about what we can do to better in messaging to our membership base to help them navigate a very complicated dynamic space around high drug costs.